Eye Examination Techniques: From Snellen Chart To Advanced Technology
The human eye is an intricate organ, essential for perceiving the world around us. Eye examinations play a pivotal role in assessing visual health and detecting potential eye disorders. Over the years, eye examination techniques have evolved significantly, from traditional methods like the Snellen chart to state-of-the-art technologies that offer precise diagnostics and personalized treatment plans. This article explores the evolution of eye examination techniques, from the conventional to the advanced, highlighting the benefits and advancements in modern ophthalmology.
The Foundation: Snellen Chart and Visual Acuity Testing
The Snellen chart, developed in the 19th century by Dutch ophthalmologist Herman Snellen, remains a cornerstone of vision testing. This chart consists of rows of letters or symbols of decreasing size, with each row corresponding to a specific visual acuity level. During a Snellen chart test, patients are asked to read the letters or symbols from a standardized distance, typically 20 feet for adults and 10 feet for children. Visual acuity is expressed as a fraction, with the numerator representing the testing distance and the denominator indicating the smallest line read correctly.
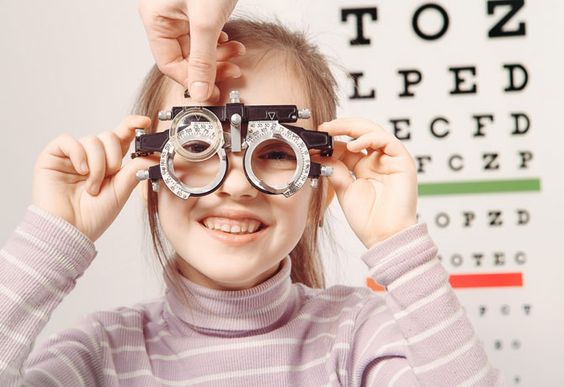
Refraction Testing: Objective and Subjective Methods
Refraction testing is crucial for determining the refractive error of the eye, including nearsightedness (myopia), farsightedness (hyperopia), and astigmatism. Objective refraction techniques, such as autorefraction and retinoscopy, provide initial measurements of refractive error without requiring patient feedback. Subjective refraction, on the other hand, involves using trial lenses and patient feedback to refine the prescription for corrective lenses. Advanced autorefractors utilize wavefront technology to provide a more detailed analysis of ocular aberrations, leading to more accurate prescriptions.
Intraocular Pressure Measurement: Tonometry Techniques
Elevated intraocular pressure (IOP) is a key risk factor for glaucoma, a leading cause of irreversible blindness. Tonometry is the standard method for measuring IOP, with the Goldmann application tonometer being the gold standard. This technique involves flattening a small area of the cornea with a calibrated probe and measuring the force required to apply the cornea. Emerging tonometry technologies, such as non-contact tonometry and rebound tonometry, offer non-invasive alternatives for IOP measurement, improving patient comfort and convenience.
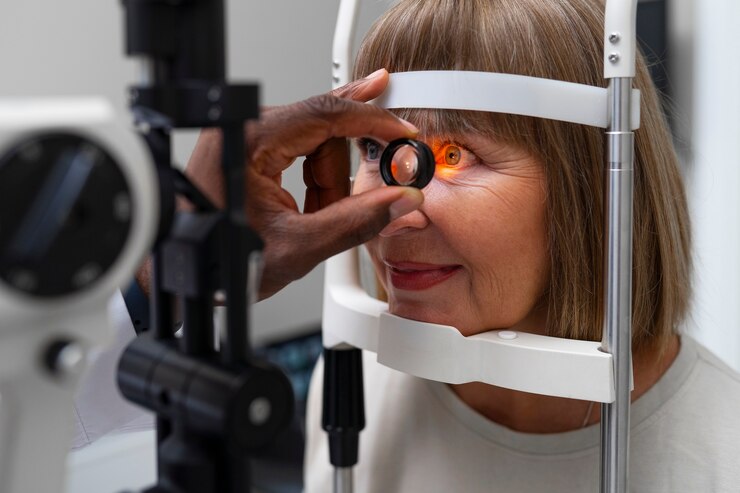
Slit-lamp Biomicroscopy: Evaluating Anterior Segment Structures
Slit-lamp biomicroscopy enables detailed examination of the anterior segment structures of the eye, including the cornea, iris, and lens. This instrument combines a binocular microscope with an adjustable slit beam of light, allowing ophthalmologists to visualize ocular structures in high resolution. Slit-lamp biomicroscopy is essential for diagnosing and monitoring various eye conditions, such as cataracts, corneal ulcers, and uveitis. Recent advancements in slit-lamp technology include digital imaging systems and integrated anterior segment optical coherence tomography (OCT), enhancing diagnostic capabilities and facilitating telemedicine consultations.
Fundus Examination: Assessing the Retina and Optic Nerve
Fundus examination involves evaluating the posterior segment of the eye, including the retina, optic nerve, and macula. Direct ophthalmoscopy and indirect ophthalmoscopy are traditional techniques used to visualize the fundus, with the latter providing a wider field of view and better stereopsis. Digital retinal imaging and fundus photography have revolutionized fundus examination, enabling non-invasive documentation of retinal pathology and facilitating remote interpretation by specialists. Optical coherence tomography (OCT) is another advanced imaging modality that provides cross-sectional images of retinal layers, aiding in the diagnosis and management of macular diseases such as age-related macular degeneration and diabetic retinopathy.
Advanced Imaging Modalities: Optical Coherence Tomography (OCT) and Beyond
Optical coherence tomography (OCT) has emerged as a cornerstone of modern ophthalmic imaging, offering high-resolution, cross-sectional visualization of ocular structures. OCT utilizes low-coherence interferometry to generate detailed images of the retina, optic nerve, and anterior segment with micrometer-level precision. In addition to spectral-domain OCT (SD-OCT), newer modalities such as swept-source OCT (SS-OCT) and enhanced-depth imaging OCT (EDI-OCT) have further expanded imaging capabilities, enabling deeper penetration and improved visualization of choroidal and scleral structures. OCT angiography (OCTA) is a non-invasive imaging technique that provides detailed visualization of retinal and choroidal vasculature, aiding in the diagnosis and monitoring of retinal vascular diseases.
Conclusion
From the humble beginnings of the Snellen chart to the sophisticated imaging technologies of today, eye examination techniques have undergone remarkable advancements, revolutionizing the field of ophthalmology. These innovations have not only improved diagnostic accuracy and patient outcomes but have also paved the way for personalized treatment strategies tailored to individual patient needs. As technology continues to evolve, the future of eye care holds great promise, offering new opportunities for early detection, intervention, and preservation of vision.