Advances In Technology For Repairing Previous Eye Surgeries
The field of ophthalmology has witnessed remarkable advancements in recent years, particularly in the realm of repairing complications from previous eye surgeries. From innovative surgical techniques to cutting-edge biomedical devices, technology has revolutionized the way surgeons approach repairing post-surgical complications. This article explores some of the most promising advances in technology for repairing previous eye surgeries, highlighting their impact on patient outcomes and quality of life.
Understanding the Need for Repair
Before delving into the advancements in technology, it’s essential to understand the common complications that may arise from previous eye surgeries. These complications can include corneal scarring, retinal detachment, glaucoma, and cataract formation, among others. Each of these complications requires specialized approaches for repair, often involving intricate surgical procedures and precise interventions.
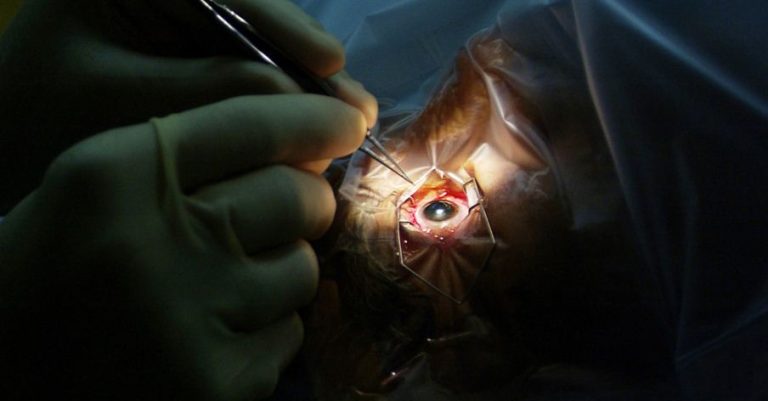
Minimally Invasive Surgical Techniques
One of the most significant advancements in repairing complications from previous eye surgeries is the development of minimally invasive surgical techniques. These techniques, such as microincisional vitrectomy surgery (MIVS) and laser-assisted procedures, offer several advantages over traditional open surgeries. They typically involve smaller incisions, reduced trauma to surrounding tissues, faster recovery times, and lower rates of complications. Minimally invasive approaches are particularly beneficial for repairing conditions such as retinal detachment and vitreous hemorrhage following previous eye surgeries.
Advanced Imaging Technologies
Another crucial aspect of repairing previous eye surgeries is accurate preoperative assessment and planning. Advanced imaging technologies, such as optical coherence tomography (OCT) and high-resolution ultrasound, play a vital role in this process. These imaging modalities allow surgeons to visualize the structures of the eye with exceptional detail, enabling precise diagnosis of complications and strategic planning of surgical interventions. By incorporating these technologies into the preoperative workflow, surgeons can optimize outcomes and minimize the risk of complications during repair procedures.
Biomedical Devices for Tissue Regeneration
In recent years, there has been growing interest in the development of biomedical devices for promoting tissue regeneration in the eye. These devices, such as bioengineered corneal scaffolds and retinal implants, hold immense potential for repairing damage caused by previous eye surgeries. Bioengineered scaffolds can provide structural support and facilitate the regeneration of corneal tissue in cases of corneal scarring or opacity. Similarly, retinal implants can restore visual function in patients with retinal degeneration or detachment following previous surgeries. While these technologies are still in the early stages of development, they represent promising avenues for future research and clinical application.
Nanotechnology and Drug Delivery Systems
Nanotechnology has emerged as a powerful tool in repairing complications from previous eye surgeries, particularly in the realm of drug delivery. Nanoparticle-based drug delivery systems offer several advantages, including enhanced drug stability, prolonged release kinetics, and targeted delivery to specific ocular tissues. These systems can be utilized to administer therapeutic agents, such as anti-inflammatory drugs or growth factors, directly to the site of injury or repair. By harnessing the potential of nanotechnology, researchers aim to improve the efficacy and safety of pharmacological interventions for managing post-surgical complications in the eye.
Telemedicine and Remote Monitoring
In addition to surgical interventions and biomedical devices, technology has also transformed the way patients receive care and follow-up after eye surgeries. Telemedicine platforms and remote monitoring systems enable patients to communicate with their healthcare providers, undergo virtual consultations, and receive personalized care plans from the comfort of their homes. These technologies are particularly beneficial for elderly or immobile patients who may have difficulty accessing traditional healthcare facilities. By facilitating remote monitoring and follow-up, telemedicine helps ensure continuity of care and early detection of complications, ultimately improving patient outcomes and satisfaction.
Conclusion
Advances in technology have revolutionized the field of ophthalmology, particularly in repairing complications from previous eye surgeries. From minimally invasive surgical techniques to advanced imaging modalities and biomedical devices, these advancements offer new hope for patients facing post-surgical complications. By embracing these technologies and incorporating them into clinical practice, ophthalmologists can optimize outcomes, enhance patient satisfaction, and continue to push the boundaries of innovation in eye surgery repair.